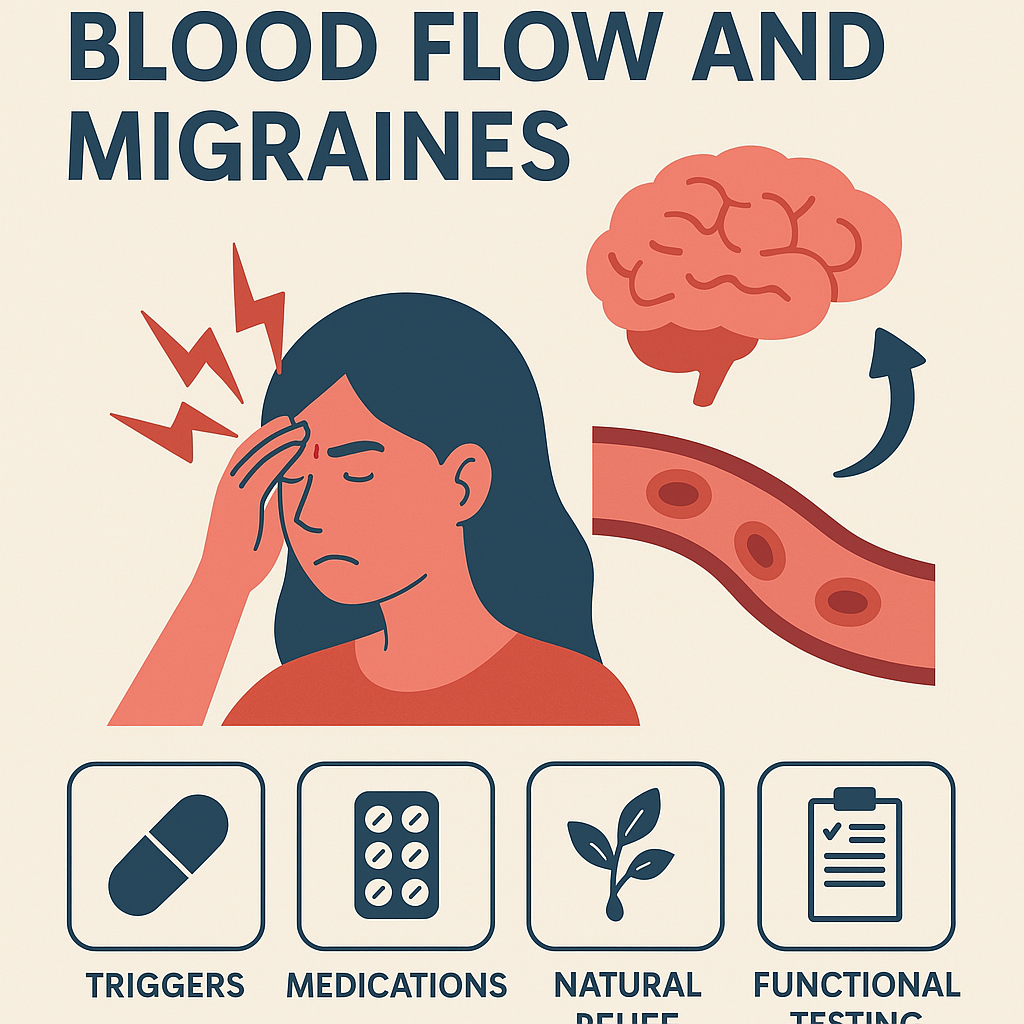
Let’s analyze common issues with migraines
Migraines are more than just headaches. They can derail your day, cloud your focus, and leave you searching for answers that feel just out of reach. While medications can offer relief, they don’t always get to the why. Why do migraines happen in the first place? And why do they keep coming back?
At Mindful Objective, we believe in looking at the whole picture—especially when it comes to complex health challenges like migraines. In Episode 12 of our podcast, we explore the often-overlooked link between blood flow and migraines, and how everything from medications to supplements to food and exercise can influence your symptoms—for better or worse.
In this post, we’re breaking down the core ideas from that episode. For a deeper dive and real-world examples, be sure to check out the full podcast on Apple, Spotify, Amazon Music, Pandora, or YouTube.
Blood Flow: The Hidden Thread in Migraines
Most people think migraines start in the head—and they do, but not in the way you might expect.
One of the most significant factors in migraines is something called cortical spreading depression—an electrical wave that slowly moves across the brain, temporarily reducing blood flow in its path. Your body senses the drop and rushes to compensate, dilating vessels to bring blood back. That overcorrection? It’s what triggers the pounding, throbbing pain many associate with migraines.
This isn’t just happening in your brain. Blood flow changes can extend into the neck, shoulders, even the eyes. If you’ve experienced migraine auras—flashes of light, visual zigzags, or blind spots—that’s likely the result of early vessel constriction before the pain sets in.
So why do these blood vessels get so reactive in the first place?
Triggers: More Than Just Stress or Wine
Common triggers like stress, lack of sleep, and certain foods don’t act alone—they interact with your internal environment. At Mindful Objective, we look at five key areas through the lens of functional lab testing:
-
Food Sensitivities: Even without digestive symptoms, foods like gluten or dairy may cause immune responses that increase inflammation and blood vessel instability.
-
Gut Imbalances: An overgrowth of bad bacteria or yeast can release toxins that ramp up inflammation and interfere with blood flow regulation.
-
Hormone Fluctuations: Estrogen dips (like during menstruation or perimenopause) can suddenly dilate blood vessels. Cortisol, your stress hormone, can stiffen vessels over time.
-
Heavy Metals: Exposure to things like mercury or lead can impair nerve signals and vascular function.
-
Nutrient Deficiencies: Low levels of magnesium, B2, or CoQ10 can leave your body less capable of controlling nerve and vessel activity under stress.
Understanding your body’s response to these factors helps move you beyond symptom management into root cause discovery.
Medications: Tools, but Not Always the Solution
Medications like Nurtec and Naratriptan have been game-changers for many. Nurtec blocks CGRP, a protein that causes vessel dilation and inflammation. Naratriptan helps reverse those effects once a migraine is underway.
But not everyone responds well. Why?
Sometimes the problem isn’t the medication—it’s the terrain it’s working in. If your gut is inflamed, your hormones are off, or your liver is struggling to detox, even helpful meds can cause unpredictable reactions. Some may stop working. Others may trigger side effects like dizziness, nausea, or rebound headaches.
At Mindful Objective, we help people use medications more effectively by understanding their unique biology. That way, your medication becomes a bridge—not a crutch—while you work on healing the deeper imbalances.
Supplements and Food: Double-Edged Swords
Natural tools can be powerful—if they’re used wisely.
Take magnesium, for instance. It relaxes blood vessels and calms nerves, which is why many migraine sufferers swear by it. But take too much, or use the wrong form, and it can lower your blood pressure or overly relax your muscles, triggering symptoms instead of relieving them.
CoQ10, riboflavin (B2), and omega-3s also show promise. They support energy production and blood flow regulation—critical in migraine prevention. But they don’t act like quick fixes. You need to be consistent and tuned in to how your body reacts.
When it comes to food, common triggers include:
-
Dark chocolate – rich in magnesium but also tyramine
-
Red wine – full of antioxidants but high in histamines and sulfites
-
Caffeine – helpful in small amounts, disastrous if overused or suddenly cut
Through food sensitivity testing and symptom tracking, we help clients move from guessing to precision-based nutrition, avoiding the unnecessary fear of entire food groups and focusing instead on personal patterns.
Exercise: Friend or Foe?
Exercise is often overlooked—but it’s a powerful modulator of blood flow. While regular movement can reduce migraine frequency, the wrong kind of activity at the wrong time can be a trigger.
High-intensity workouts or sudden heavy lifting can spike blood pressure and trigger a migraine in sensitive people. On the flip side, gentle practices like yoga, walking, or tai chi can help regulate circulation and reduce inflammation.
The key? Understand your baseline and build tolerance slowly. Start with short, low-impact sessions. Monitor hydration, sleep, and stress levels before exercising. Consider preemptive support—some use medications like Nurtec before high-exertion days to prevent flare-ups.
As always, functional testing helps clarify why exercise triggers you. Low iron? Gut inflammation? Adrenal imbalances? When you know the root, you can design an approach that actually works for you.
Ready to Go Deeper?
Migraines don’t happen in a vacuum. They’re a response to how your brain, blood vessels, hormones, nervous system, and immune system are communicating. When one of those systems is out of sync, migraines are often the body’s signal that something needs attention.
You don’t have to figure this out alone. We’re here to help you connect the dots—between triggers, biology, and relief.
For the full breakdown—including how we support people through lab testing, custom strategies, and integrative support—tune into Episode 12 of Mindful Objective.
🎧 Listen now on your favorite platform:
Migraines are complex—but you’re not broken. Your body is communicating. Let’s figure out what it’s trying to say.
We’re here to help you connect the dots, understand what your body needs, and create a realistic plan for long-term wellness. At Mindful Objective, your health isn’t just a goal—it’s a foundation for everything else.
Want to learn more or get started? Check Us Out!
This is for informational and educational purposes only. We do not diagnose, cure, or treat any illness or disease.
🧠 References
-
Cortical spreading depression as a target for anti-migraine agents
https://doi.org/10.1111/j.1526-4610.2010.01775.x -
Calcitonin Gene-Related Peptide (CGRP) and Migraine: From Bench to Bedside
https://doi.org/10.1111/head.13301 -
Migraine prophylaxis: A randomized controlled trial of magnesium
https://doi.org/10.1046/j.1468-2982.1996.1604312.x -
Migraine and reproductive hormones throughout the life cycle
https://doi.org/10.1016/S1474-4422(04)00735-5 -
The Gut–Brain Axis: A Missing Link in Depression
https://doi.org/10.3389/fpsyt.2015.00064